The Africa CDC Equation in Africa’s Health
March 17, 2023
By Ajong Mbapndah L
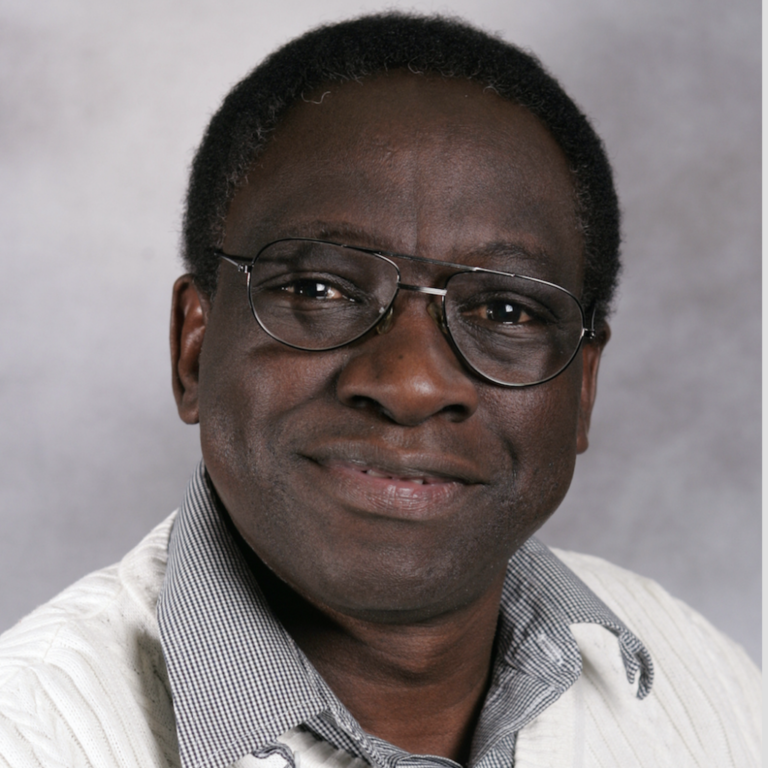
[caption id="attachment_105208" align="alignnone" width="1080"] Africa CDC remains resolute in achieving its goal of safeguarding Africa’s health, says Dr Benjamin Djoudalbaye[/caption]
Established in January 2016 by the 26th Ordinary Assembly of Heads of State and Government and officially launched in January 2017, Africa CDC has wasted little time in establishing itself as a leader on health care issues across the continent.
In a bid to get more insights into its mission and perspectives, PAV caught up with Dr Benjamin Djoudalbaye, Interim Coordinator for Central Africa and Head of Policy and Diplomacy and Communication at Africa CDC. Despite the many challenges faced by the health systems across the continent, Africa CDC remains resolute in achieving its goal of safeguarding Africa’s health, says Dr Djoudalbaye.
Could we start with an overview of how Africa CDC has fared since it went operational some six years ago?
Dr Benjamin Djoudalbaye: From an institutional perspective, I would say Africa CDC is doing very well executing the mandate given by the heads of state and government. We have a functioning instructional structure that effectively responds to Member States’ requests in times of outbreaks, which is a critical part of our work. Despite the many challenges faced by the health systems across the continent, Africa CDC remains resolute in achieving its goal of safeguarding Africa’s health.
Can you situate the overall importance or place of Africa CDC today in the African healthcare landscape?
Dr Benjamin Djoudalbaye: Looking back on how far we have come, I think Africa CDC is gradually taking place as the lead institution to drive Africa’s continental health security agenda. Africa CDC is a specialized agency of the African Union (AU), established in April 2017. Its mission is to strengthen Africa’s public health systems by improving surveillance, detection, and response to infectious diseases and providing technical guidance and capacity-building in critical areas such as laboratories. The decision by the AU Assembly in 2022 to elevate Africa CDC to an autonomous status has given the organization more leverage to implement its strategic objectives with an agenda for a New Public Health Order for Africa. This agenda focuses on strengthening public health institutions and the workforce on the continent, supporting domestic financing for health and local manufacturing, and seeking respectful and action-oriented partnerships based on Africa’s priorities.
How are the services of the CDC rendered or structured in a way that every day Africans feel its impact?
Dr Benjamin Djoudalbaye: As per the Africa CDC mandate, we work directly with Member States, with our entry point being the National Public Health Institutes (NPHIs) and the Ministries of Health in countries where the structures of NPHIs are yet to be established. This engagement with the AU Member States, I must say, is based on the specific country’s priorities and needs. Our support covers building capacities of the health workforce, strengthening Laboratory, surveillance, and other key areas within the health system.
May we know how much of a funding stake the AU and its member countries have in Africa CDC?
Dr Benjamin Djoudalbaye: Africa CDC is fully funded by the African Union Member States. Yes
The CDC got great credit from its handling of the COVID-19 pandemic, what are some of the major lessons learned as an institution and what policy recommendations for African countries to better prepare for future pandemics?
Dr Benjamin Djoudalbaye: The pandemic has caused immense disruption to African countries, particularly those already crisis ridden.
Lesson 1: Preparedness is crucial
The COVID-19 pandemic showed that being prepared is essential in a global health crisis. Many African countries were ill-prepared, with limited healthcare facilities and resources to cope with the pandemic. This has highlighted the need for African countries to develop comprehensive and comprehensive plans for dealing with any future health or economic crisis. Countries must also be prepared to take rapid and decisive action when faced with a new health crisis, rather than relying on international support.
Lesson 2: Strengthening Health Systems
The pandemic has shown the importance of strengthening health systems and investing in health care to respond to future pandemics. Many African countries have insufficient healthcare infrastructure and resources, making it difficult to respond to the pandemic. Sub-Saharan countries, in particular were already dealing with the burden of diseases such as malaria, HIV/AIDS, and tuberculosis, and the pandemic revealed the urgent need to invest more in healthcare systems in Africa. This means increasing investment in public health and primary healthcare services, which could help to improve access to medicines and vaccines and reduce health inequalities.
Lesson 3: Promoting Health Security
African countries should take steps to promote health security by investing in research, preparedness and surveillance. This can be done by strengthening international health regulations to ensure African countries are better equipped to detect and respond to public health threats. This includes increasing resourcing and capacity building at national and regional levels and supporting collaborations between African countries for rapid response.
Lesson 4: Strengthening Collaboration
The pandemic highlighted the importance of international collaboration, from sharing best practices to ensure equitable access to tests and treatments. This demonstrated the need for African countries to strengthen their cooperation and collaboration with each other and international partners.
These lessons highlight the need for long-term, comprehensive and comprehensive strategies, even in the wake of a pandemic. In the wake of Covid-19, governments in Africa must proactively invest in public health systems, economic transformation and efforts to reduce inequality, and undertake additional measures to ensure the resilience of country populations and society.
[caption id="attachment_105209" align="alignnone" width="1080"]
Africa CDC remains resolute in achieving its goal of safeguarding Africa’s health, says Dr Benjamin Djoudalbaye[/caption]
Established in January 2016 by the 26th Ordinary Assembly of Heads of State and Government and officially launched in January 2017, Africa CDC has wasted little time in establishing itself as a leader on health care issues across the continent.
In a bid to get more insights into its mission and perspectives, PAV caught up with Dr Benjamin Djoudalbaye, Interim Coordinator for Central Africa and Head of Policy and Diplomacy and Communication at Africa CDC. Despite the many challenges faced by the health systems across the continent, Africa CDC remains resolute in achieving its goal of safeguarding Africa’s health, says Dr Djoudalbaye.
Could we start with an overview of how Africa CDC has fared since it went operational some six years ago?
Dr Benjamin Djoudalbaye: From an institutional perspective, I would say Africa CDC is doing very well executing the mandate given by the heads of state and government. We have a functioning instructional structure that effectively responds to Member States’ requests in times of outbreaks, which is a critical part of our work. Despite the many challenges faced by the health systems across the continent, Africa CDC remains resolute in achieving its goal of safeguarding Africa’s health.
Can you situate the overall importance or place of Africa CDC today in the African healthcare landscape?
Dr Benjamin Djoudalbaye: Looking back on how far we have come, I think Africa CDC is gradually taking place as the lead institution to drive Africa’s continental health security agenda. Africa CDC is a specialized agency of the African Union (AU), established in April 2017. Its mission is to strengthen Africa’s public health systems by improving surveillance, detection, and response to infectious diseases and providing technical guidance and capacity-building in critical areas such as laboratories. The decision by the AU Assembly in 2022 to elevate Africa CDC to an autonomous status has given the organization more leverage to implement its strategic objectives with an agenda for a New Public Health Order for Africa. This agenda focuses on strengthening public health institutions and the workforce on the continent, supporting domestic financing for health and local manufacturing, and seeking respectful and action-oriented partnerships based on Africa’s priorities.
How are the services of the CDC rendered or structured in a way that every day Africans feel its impact?
Dr Benjamin Djoudalbaye: As per the Africa CDC mandate, we work directly with Member States, with our entry point being the National Public Health Institutes (NPHIs) and the Ministries of Health in countries where the structures of NPHIs are yet to be established. This engagement with the AU Member States, I must say, is based on the specific country’s priorities and needs. Our support covers building capacities of the health workforce, strengthening Laboratory, surveillance, and other key areas within the health system.
May we know how much of a funding stake the AU and its member countries have in Africa CDC?
Dr Benjamin Djoudalbaye: Africa CDC is fully funded by the African Union Member States. Yes
The CDC got great credit from its handling of the COVID-19 pandemic, what are some of the major lessons learned as an institution and what policy recommendations for African countries to better prepare for future pandemics?
Dr Benjamin Djoudalbaye: The pandemic has caused immense disruption to African countries, particularly those already crisis ridden.
Lesson 1: Preparedness is crucial
The COVID-19 pandemic showed that being prepared is essential in a global health crisis. Many African countries were ill-prepared, with limited healthcare facilities and resources to cope with the pandemic. This has highlighted the need for African countries to develop comprehensive and comprehensive plans for dealing with any future health or economic crisis. Countries must also be prepared to take rapid and decisive action when faced with a new health crisis, rather than relying on international support.
Lesson 2: Strengthening Health Systems
The pandemic has shown the importance of strengthening health systems and investing in health care to respond to future pandemics. Many African countries have insufficient healthcare infrastructure and resources, making it difficult to respond to the pandemic. Sub-Saharan countries, in particular were already dealing with the burden of diseases such as malaria, HIV/AIDS, and tuberculosis, and the pandemic revealed the urgent need to invest more in healthcare systems in Africa. This means increasing investment in public health and primary healthcare services, which could help to improve access to medicines and vaccines and reduce health inequalities.
Lesson 3: Promoting Health Security
African countries should take steps to promote health security by investing in research, preparedness and surveillance. This can be done by strengthening international health regulations to ensure African countries are better equipped to detect and respond to public health threats. This includes increasing resourcing and capacity building at national and regional levels and supporting collaborations between African countries for rapid response.
Lesson 4: Strengthening Collaboration
The pandemic highlighted the importance of international collaboration, from sharing best practices to ensure equitable access to tests and treatments. This demonstrated the need for African countries to strengthen their cooperation and collaboration with each other and international partners.
These lessons highlight the need for long-term, comprehensive and comprehensive strategies, even in the wake of a pandemic. In the wake of Covid-19, governments in Africa must proactively invest in public health systems, economic transformation and efforts to reduce inequality, and undertake additional measures to ensure the resilience of country populations and society.
[caption id="attachment_105209" align="alignnone" width="1080"] In the wake of Covid-19, governments in Africa must proactively invest in public health systems, economic transformation and efforts to reduce inequality, says Dr Djoudalbaye[/caption]
May we know some of the primary healthcare issues facing the continent?
Dr Benjamin Djoudalbaye: Access to Quality Health Care: A major healthcare issue facing Africa is the lack of access to quality and affordable health care. With limited resources and infrastructure, many countries in the continent cannot provide adequate health services to their population. Furthermore, even when affordable healthcare is available, it is often of poor quality or unavailable in remote or rural areas.
- HIV/AIDS and Other Infectious Diseases: HIV/AIDS is a major public health challenge in the African continent. Although rates of HIV transmission have decreased over the years, the disease is still a major cause of mortality in many countries. Other infectious diseases such as malaria, tuberculosis and schistosomiasis and other Neglected Tropical Diseases are also major issues, and continued efforts to control and prevent their spread is critical to improving the population's overall health.
Non-communicable diseases such as cardiovascular diseases, diabetes, cancer and chronic respiratory diseases are also the leading causes of death and disability in Africa.
In the wake of Covid-19, governments in Africa must proactively invest in public health systems, economic transformation and efforts to reduce inequality, says Dr Djoudalbaye[/caption]
May we know some of the primary healthcare issues facing the continent?
Dr Benjamin Djoudalbaye: Access to Quality Health Care: A major healthcare issue facing Africa is the lack of access to quality and affordable health care. With limited resources and infrastructure, many countries in the continent cannot provide adequate health services to their population. Furthermore, even when affordable healthcare is available, it is often of poor quality or unavailable in remote or rural areas.
- HIV/AIDS and Other Infectious Diseases: HIV/AIDS is a major public health challenge in the African continent. Although rates of HIV transmission have decreased over the years, the disease is still a major cause of mortality in many countries. Other infectious diseases such as malaria, tuberculosis and schistosomiasis and other Neglected Tropical Diseases are also major issues, and continued efforts to control and prevent their spread is critical to improving the population's overall health.
Non-communicable diseases such as cardiovascular diseases, diabetes, cancer and chronic respiratory diseases are also the leading causes of death and disability in Africa.
- Counterfeit Drugs: Counterfeit drugs are another major healthcare issue facing Africa. As the drugs are often cheaper than their legitimate counterparts, many people are willing to purchase them, unaware of the risks of consuming such medications. Sometimes the medicines are fake, substandard or non-existent quality and can even be dangerous to health.
- Lack of Health Insurance: Many countries in Africa do not have a functional healthcare insurance system, and thus, a significant number of the population is unable to access healthcare services due to financial constraints
The 36th AU Assembly of Heads of State and Governments ended recently, how did the CDC feature in the deliberations and any major policy decisions or orientations?
Dr Benjamin Djoudalbaye: Our major outcome was the new Director General appointment by Heads of State and Government as the Chief Executive Officer. He will be responsible for the overall management of the Africa CDC.
What kind of relations does the CDC have with other international bodies operating in the continent, like the WHO?
Dr Benjamin Djoudalbaye: Africa CDC has a very close working relationship with international bodies operating in Africa. With WHO, we collaborate on many programmes across the continent, providing technical support to Member States.
[caption id="attachment_105210" align="alignnone" width="1080"]

For Dr Djoudalbaye, African countries should take steps to promote health security by investing in research, preparedness and surveillance.[/caption]
What are some of the most serious challenges the CDC has faced in the implementation of its programs across the continent?
The challenges are not different from what I mentioned earlier. I can cite the following:
- A lack of finances, medical equipment, and medical personnel challenges the African health system. This has left some parts of Africa with insufficient resources to provide essential healthcare services adequately.
- Many African countries suffer from poor infrastructure that hinders the delivery of essential healthcare services. Poor roads, limited access to clean water, and inadequate electricity contribute to the poor delivery of healthcare resources in Africa.
- Despite improvements in recent years, many African countries still lack access to healthcare services. Barriers such as geographical distance or financial instability prevent individuals from accessing vital healthcare services.
-African healthcare systems often suffer from poor quality of care. Low pay for healthcare workers, a lack of training, or drug shortages contribute to inadequate quality of care in African nations.
-Non-communicable diseases significantly contribute to death in Africa, yet they are often not given adequate attention. This is due to the focus of healthcare systems on infectious diseases such as HIV/AIDS, TB and malaria, which receive the bulk of medical funding.
For 2023, what are some of the major projects that the CDC will be working on?
Dr Benjamin Djoudalbaye: I will talk about priorities rather than projects. We will continue supporting the African Union Member States in the following areas:
-Strengthen health-related surveillance systems for improved public health decision-making and action.
-Develop and strengthen information systems that inform and support African public health needs and actions.
-Ensure effective public health emergency preparedness and response capabilities
-Strengthen public health institutions and improve evidence-based decision-making and practice.
-Strengthen Africa’s clinical and public health laboratory systems and networks.
**
Culled from
March Issue of
PAV Magazine


 Africa CDC remains resolute in achieving its goal of safeguarding Africa’s health, says Dr Benjamin Djoudalbaye[/caption]
Established in January 2016 by the 26th Ordinary Assembly of Heads of State and Government and officially launched in January 2017, Africa CDC has wasted little time in establishing itself as a leader on health care issues across the continent.
In a bid to get more insights into its mission and perspectives, PAV caught up with Dr Benjamin Djoudalbaye, Interim Coordinator for Central Africa and Head of Policy and Diplomacy and Communication at Africa CDC. Despite the many challenges faced by the health systems across the continent, Africa CDC remains resolute in achieving its goal of safeguarding Africa’s health, says Dr Djoudalbaye.
Could we start with an overview of how Africa CDC has fared since it went operational some six years ago?
Dr Benjamin Djoudalbaye: From an institutional perspective, I would say Africa CDC is doing very well executing the mandate given by the heads of state and government. We have a functioning instructional structure that effectively responds to Member States’ requests in times of outbreaks, which is a critical part of our work. Despite the many challenges faced by the health systems across the continent, Africa CDC remains resolute in achieving its goal of safeguarding Africa’s health.
Can you situate the overall importance or place of Africa CDC today in the African healthcare landscape?
Dr Benjamin Djoudalbaye: Looking back on how far we have come, I think Africa CDC is gradually taking place as the lead institution to drive Africa’s continental health security agenda. Africa CDC is a specialized agency of the African Union (AU), established in April 2017. Its mission is to strengthen Africa’s public health systems by improving surveillance, detection, and response to infectious diseases and providing technical guidance and capacity-building in critical areas such as laboratories. The decision by the AU Assembly in 2022 to elevate Africa CDC to an autonomous status has given the organization more leverage to implement its strategic objectives with an agenda for a New Public Health Order for Africa. This agenda focuses on strengthening public health institutions and the workforce on the continent, supporting domestic financing for health and local manufacturing, and seeking respectful and action-oriented partnerships based on Africa’s priorities.
How are the services of the CDC rendered or structured in a way that every day Africans feel its impact?
Dr Benjamin Djoudalbaye: As per the Africa CDC mandate, we work directly with Member States, with our entry point being the National Public Health Institutes (NPHIs) and the Ministries of Health in countries where the structures of NPHIs are yet to be established. This engagement with the AU Member States, I must say, is based on the specific country’s priorities and needs. Our support covers building capacities of the health workforce, strengthening Laboratory, surveillance, and other key areas within the health system.
May we know how much of a funding stake the AU and its member countries have in Africa CDC?
Dr Benjamin Djoudalbaye: Africa CDC is fully funded by the African Union Member States. Yes
The CDC got great credit from its handling of the COVID-19 pandemic, what are some of the major lessons learned as an institution and what policy recommendations for African countries to better prepare for future pandemics?
Dr Benjamin Djoudalbaye: The pandemic has caused immense disruption to African countries, particularly those already crisis ridden.
Lesson 1: Preparedness is crucial
The COVID-19 pandemic showed that being prepared is essential in a global health crisis. Many African countries were ill-prepared, with limited healthcare facilities and resources to cope with the pandemic. This has highlighted the need for African countries to develop comprehensive and comprehensive plans for dealing with any future health or economic crisis. Countries must also be prepared to take rapid and decisive action when faced with a new health crisis, rather than relying on international support.
Lesson 2: Strengthening Health Systems
The pandemic has shown the importance of strengthening health systems and investing in health care to respond to future pandemics. Many African countries have insufficient healthcare infrastructure and resources, making it difficult to respond to the pandemic. Sub-Saharan countries, in particular were already dealing with the burden of diseases such as malaria, HIV/AIDS, and tuberculosis, and the pandemic revealed the urgent need to invest more in healthcare systems in Africa. This means increasing investment in public health and primary healthcare services, which could help to improve access to medicines and vaccines and reduce health inequalities.
Lesson 3: Promoting Health Security
African countries should take steps to promote health security by investing in research, preparedness and surveillance. This can be done by strengthening international health regulations to ensure African countries are better equipped to detect and respond to public health threats. This includes increasing resourcing and capacity building at national and regional levels and supporting collaborations between African countries for rapid response.
Lesson 4: Strengthening Collaboration
The pandemic highlighted the importance of international collaboration, from sharing best practices to ensure equitable access to tests and treatments. This demonstrated the need for African countries to strengthen their cooperation and collaboration with each other and international partners.
These lessons highlight the need for long-term, comprehensive and comprehensive strategies, even in the wake of a pandemic. In the wake of Covid-19, governments in Africa must proactively invest in public health systems, economic transformation and efforts to reduce inequality, and undertake additional measures to ensure the resilience of country populations and society.
[caption id="attachment_105209" align="alignnone" width="1080"]
Africa CDC remains resolute in achieving its goal of safeguarding Africa’s health, says Dr Benjamin Djoudalbaye[/caption]
Established in January 2016 by the 26th Ordinary Assembly of Heads of State and Government and officially launched in January 2017, Africa CDC has wasted little time in establishing itself as a leader on health care issues across the continent.
In a bid to get more insights into its mission and perspectives, PAV caught up with Dr Benjamin Djoudalbaye, Interim Coordinator for Central Africa and Head of Policy and Diplomacy and Communication at Africa CDC. Despite the many challenges faced by the health systems across the continent, Africa CDC remains resolute in achieving its goal of safeguarding Africa’s health, says Dr Djoudalbaye.
Could we start with an overview of how Africa CDC has fared since it went operational some six years ago?
Dr Benjamin Djoudalbaye: From an institutional perspective, I would say Africa CDC is doing very well executing the mandate given by the heads of state and government. We have a functioning instructional structure that effectively responds to Member States’ requests in times of outbreaks, which is a critical part of our work. Despite the many challenges faced by the health systems across the continent, Africa CDC remains resolute in achieving its goal of safeguarding Africa’s health.
Can you situate the overall importance or place of Africa CDC today in the African healthcare landscape?
Dr Benjamin Djoudalbaye: Looking back on how far we have come, I think Africa CDC is gradually taking place as the lead institution to drive Africa’s continental health security agenda. Africa CDC is a specialized agency of the African Union (AU), established in April 2017. Its mission is to strengthen Africa’s public health systems by improving surveillance, detection, and response to infectious diseases and providing technical guidance and capacity-building in critical areas such as laboratories. The decision by the AU Assembly in 2022 to elevate Africa CDC to an autonomous status has given the organization more leverage to implement its strategic objectives with an agenda for a New Public Health Order for Africa. This agenda focuses on strengthening public health institutions and the workforce on the continent, supporting domestic financing for health and local manufacturing, and seeking respectful and action-oriented partnerships based on Africa’s priorities.
How are the services of the CDC rendered or structured in a way that every day Africans feel its impact?
Dr Benjamin Djoudalbaye: As per the Africa CDC mandate, we work directly with Member States, with our entry point being the National Public Health Institutes (NPHIs) and the Ministries of Health in countries where the structures of NPHIs are yet to be established. This engagement with the AU Member States, I must say, is based on the specific country’s priorities and needs. Our support covers building capacities of the health workforce, strengthening Laboratory, surveillance, and other key areas within the health system.
May we know how much of a funding stake the AU and its member countries have in Africa CDC?
Dr Benjamin Djoudalbaye: Africa CDC is fully funded by the African Union Member States. Yes
The CDC got great credit from its handling of the COVID-19 pandemic, what are some of the major lessons learned as an institution and what policy recommendations for African countries to better prepare for future pandemics?
Dr Benjamin Djoudalbaye: The pandemic has caused immense disruption to African countries, particularly those already crisis ridden.
Lesson 1: Preparedness is crucial
The COVID-19 pandemic showed that being prepared is essential in a global health crisis. Many African countries were ill-prepared, with limited healthcare facilities and resources to cope with the pandemic. This has highlighted the need for African countries to develop comprehensive and comprehensive plans for dealing with any future health or economic crisis. Countries must also be prepared to take rapid and decisive action when faced with a new health crisis, rather than relying on international support.
Lesson 2: Strengthening Health Systems
The pandemic has shown the importance of strengthening health systems and investing in health care to respond to future pandemics. Many African countries have insufficient healthcare infrastructure and resources, making it difficult to respond to the pandemic. Sub-Saharan countries, in particular were already dealing with the burden of diseases such as malaria, HIV/AIDS, and tuberculosis, and the pandemic revealed the urgent need to invest more in healthcare systems in Africa. This means increasing investment in public health and primary healthcare services, which could help to improve access to medicines and vaccines and reduce health inequalities.
Lesson 3: Promoting Health Security
African countries should take steps to promote health security by investing in research, preparedness and surveillance. This can be done by strengthening international health regulations to ensure African countries are better equipped to detect and respond to public health threats. This includes increasing resourcing and capacity building at national and regional levels and supporting collaborations between African countries for rapid response.
Lesson 4: Strengthening Collaboration
The pandemic highlighted the importance of international collaboration, from sharing best practices to ensure equitable access to tests and treatments. This demonstrated the need for African countries to strengthen their cooperation and collaboration with each other and international partners.
These lessons highlight the need for long-term, comprehensive and comprehensive strategies, even in the wake of a pandemic. In the wake of Covid-19, governments in Africa must proactively invest in public health systems, economic transformation and efforts to reduce inequality, and undertake additional measures to ensure the resilience of country populations and society.
[caption id="attachment_105209" align="alignnone" width="1080"] In the wake of Covid-19, governments in Africa must proactively invest in public health systems, economic transformation and efforts to reduce inequality, says Dr Djoudalbaye[/caption]
May we know some of the primary healthcare issues facing the continent?
Dr Benjamin Djoudalbaye: Access to Quality Health Care: A major healthcare issue facing Africa is the lack of access to quality and affordable health care. With limited resources and infrastructure, many countries in the continent cannot provide adequate health services to their population. Furthermore, even when affordable healthcare is available, it is often of poor quality or unavailable in remote or rural areas.
- HIV/AIDS and Other Infectious Diseases: HIV/AIDS is a major public health challenge in the African continent. Although rates of HIV transmission have decreased over the years, the disease is still a major cause of mortality in many countries. Other infectious diseases such as malaria, tuberculosis and schistosomiasis and other Neglected Tropical Diseases are also major issues, and continued efforts to control and prevent their spread is critical to improving the population's overall health.
Non-communicable diseases such as cardiovascular diseases, diabetes, cancer and chronic respiratory diseases are also the leading causes of death and disability in Africa.
In the wake of Covid-19, governments in Africa must proactively invest in public health systems, economic transformation and efforts to reduce inequality, says Dr Djoudalbaye[/caption]
May we know some of the primary healthcare issues facing the continent?
Dr Benjamin Djoudalbaye: Access to Quality Health Care: A major healthcare issue facing Africa is the lack of access to quality and affordable health care. With limited resources and infrastructure, many countries in the continent cannot provide adequate health services to their population. Furthermore, even when affordable healthcare is available, it is often of poor quality or unavailable in remote or rural areas.
- HIV/AIDS and Other Infectious Diseases: HIV/AIDS is a major public health challenge in the African continent. Although rates of HIV transmission have decreased over the years, the disease is still a major cause of mortality in many countries. Other infectious diseases such as malaria, tuberculosis and schistosomiasis and other Neglected Tropical Diseases are also major issues, and continued efforts to control and prevent their spread is critical to improving the population's overall health.
Non-communicable diseases such as cardiovascular diseases, diabetes, cancer and chronic respiratory diseases are also the leading causes of death and disability in Africa.
 For Dr Djoudalbaye, African countries should take steps to promote health security by investing in research, preparedness and surveillance.[/caption]
What are some of the most serious challenges the CDC has faced in the implementation of its programs across the continent?
The challenges are not different from what I mentioned earlier. I can cite the following:
- A lack of finances, medical equipment, and medical personnel challenges the African health system. This has left some parts of Africa with insufficient resources to provide essential healthcare services adequately.
- Many African countries suffer from poor infrastructure that hinders the delivery of essential healthcare services. Poor roads, limited access to clean water, and inadequate electricity contribute to the poor delivery of healthcare resources in Africa.
- Despite improvements in recent years, many African countries still lack access to healthcare services. Barriers such as geographical distance or financial instability prevent individuals from accessing vital healthcare services.
-African healthcare systems often suffer from poor quality of care. Low pay for healthcare workers, a lack of training, or drug shortages contribute to inadequate quality of care in African nations.
-Non-communicable diseases significantly contribute to death in Africa, yet they are often not given adequate attention. This is due to the focus of healthcare systems on infectious diseases such as HIV/AIDS, TB and malaria, which receive the bulk of medical funding.
For 2023, what are some of the major projects that the CDC will be working on?
Dr Benjamin Djoudalbaye: I will talk about priorities rather than projects. We will continue supporting the African Union Member States in the following areas:
-Strengthen health-related surveillance systems for improved public health decision-making and action.
-Develop and strengthen information systems that inform and support African public health needs and actions.
-Ensure effective public health emergency preparedness and response capabilities
-Strengthen public health institutions and improve evidence-based decision-making and practice.
-Strengthen Africa’s clinical and public health laboratory systems and networks.
**
For Dr Djoudalbaye, African countries should take steps to promote health security by investing in research, preparedness and surveillance.[/caption]
What are some of the most serious challenges the CDC has faced in the implementation of its programs across the continent?
The challenges are not different from what I mentioned earlier. I can cite the following:
- A lack of finances, medical equipment, and medical personnel challenges the African health system. This has left some parts of Africa with insufficient resources to provide essential healthcare services adequately.
- Many African countries suffer from poor infrastructure that hinders the delivery of essential healthcare services. Poor roads, limited access to clean water, and inadequate electricity contribute to the poor delivery of healthcare resources in Africa.
- Despite improvements in recent years, many African countries still lack access to healthcare services. Barriers such as geographical distance or financial instability prevent individuals from accessing vital healthcare services.
-African healthcare systems often suffer from poor quality of care. Low pay for healthcare workers, a lack of training, or drug shortages contribute to inadequate quality of care in African nations.
-Non-communicable diseases significantly contribute to death in Africa, yet they are often not given adequate attention. This is due to the focus of healthcare systems on infectious diseases such as HIV/AIDS, TB and malaria, which receive the bulk of medical funding.
For 2023, what are some of the major projects that the CDC will be working on?
Dr Benjamin Djoudalbaye: I will talk about priorities rather than projects. We will continue supporting the African Union Member States in the following areas:
-Strengthen health-related surveillance systems for improved public health decision-making and action.
-Develop and strengthen information systems that inform and support African public health needs and actions.
-Ensure effective public health emergency preparedness and response capabilities
-Strengthen public health institutions and improve evidence-based decision-making and practice.
-Strengthen Africa’s clinical and public health laboratory systems and networks.
**